Which Preventive Service Is Offered Free Under The Aca?
A key provision of the Affordable Care Act (ACA) is the requirement that individual insurance plans comprehend recommended preventive services without any patient toll-sharing.ane Research has shown that bear witness-based preventive services tin can relieve lives and ameliorate wellness by identifying illnesses earlier, managing them more effectively, and treating them before they develop into more complicated, debilitating weather, and that some services are besides cost-effective.2 However, costs do prevent some individuals from obtaining preventive services (Figure one). The coverage requirement aims to remove cost barriers.
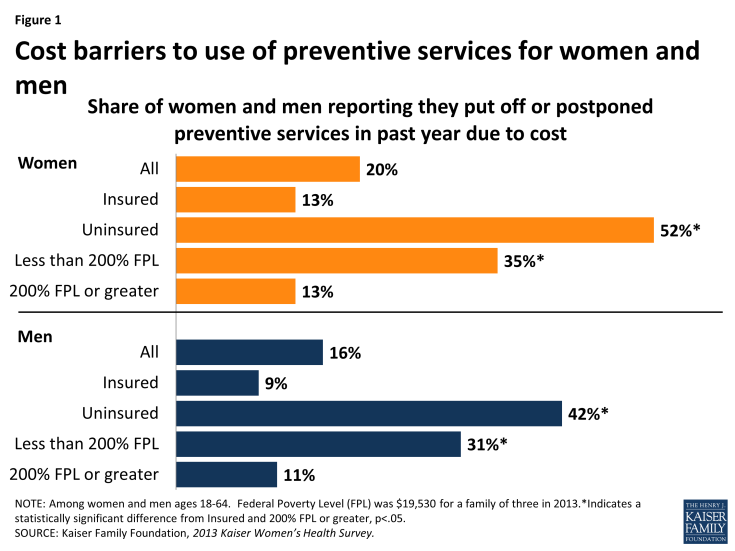
Effigy ane: Cost barriers to use of preventive services for women and men
ACA Requirements for Coverage of Preventive Services
Under Section 2713 of the ACA, private health plans must provide coverage for a range of preventive services and may not impose cost-sharing (such as copayments, deductibles, or co-insurance) on patients receiving these services. 3 These requirements utilise to all private plans – including private, small group, large group, and self-insured plans in which employers contract authoritative services to a third party payer – with the exception of those plans that maintain "grandfathered" status. In order to have been classified as "grandfathered," plans must have been in being prior to March 23, 2010, and cannot make significant changes to their coverage (for case, increasing patient price-sharing, cut benefits, or reducing employer contributions). In 2014, 26% of workers covered in employer sponsored plans were still in grandfathered plans,four and it is expected that over time almost all plans will lose their grandfathered status.
The required preventive services come up from recommendations fabricated past four expert medical and scientific bodies – the U.Due south. Preventive Services Task Force (USPSTF), the Advisory Committee on Immunization Practices (ACIP), the Health Resources and Services Administration'due south (HRSA's) Brilliant Futures Project, and HRSA and the Institute of Medicine (IOM) committee on women's clinical preventive services. The requirement that insurers comprehend preventive services recommended past the USPSTF, ACIP, and Bright Futures program went into effect for non-grandfathered plans with plan-years beginning on or afterward September 23, 2010. The coverage requirements for women's clinical preventive services became effective for plans starting on or after August 1, 2012. New or updated recommendations issued by these expert panels are required to exist covered without cost-sharing starting time in the program yr that begins on or afterward exactly one year from the latest issue appointment.five If a recommendation is changed during a programme year, an issuer is not required to make changes mid programme year, unless one of the recommending bodies determines that a service is discouraged because it is harmful or poses a significant safety concern.half-dozen In these circumstances, federal guidance will exist issued.7 Individual and minor grouping plans in the new wellness insurance marketplaces are also required to cover an essential health do good (EHB) packet – in add-on to the full range of preventive requirements described in this fact sheet. There is some crossover as several of the specific preventive services fall into the EHB categories. However, just preventive services recommended by 1 of the four groups discussed in this factsheet are covered without price-sharing.
Clinical Preventive Services for Adults and Children
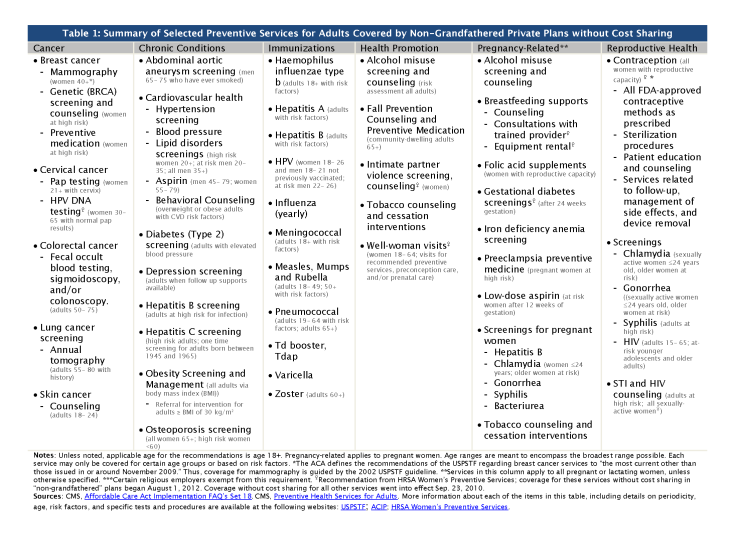
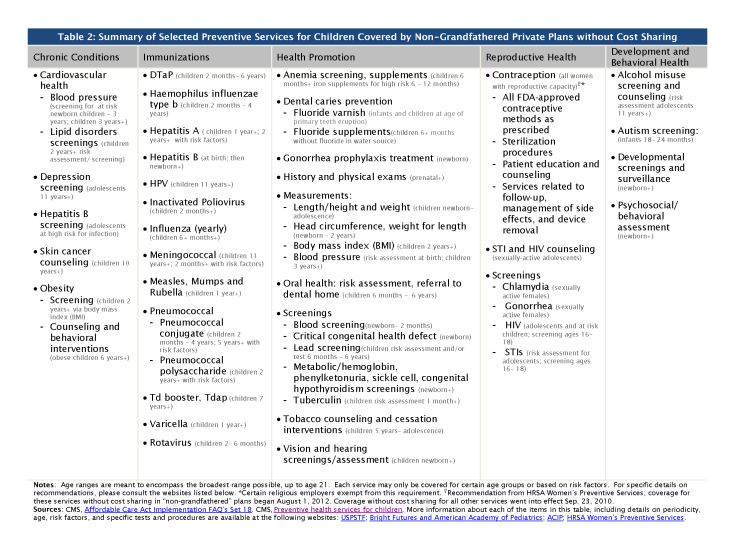
The ACA requires private plans to cover the post-obit four broad categories of services for adults and children (summarized in Tables ane and 2):
I. Evidence-Based Screenings and Counseling
Insurers now must cover show-based services for adults that have a rating of "A" or "B" in the electric current recommendations of the United States Preventive Services Chore Forcefulness (USPSTF), an independent panel of clinicians and scientists commissioned past the Bureau for Healthcare Research and Quality. An "A" or "B" letter grade indicates that the console finds there is high certainty that the services have a substantial or moderate net benefit. The services required to be covered without cost-sharing include screening for depression, diabetes, cholesterol, obesity, various cancers, HIV and sexually transmitted infections (STIs), also as counseling for drug and tobacco use, salubrious eating, and other mutual health concerns. The consequence date for a recommendation from USPTF is considered to be the last twenty-four hours of the month in which it is published or otherwise released.
Ii. Routine Immunizations
Health plans must also provide coverage without cost-sharing for immunizations that are recommended and determined to exist for routine utilize by the Informational Commission on Immunization Practices (ACIP), a federal committee comprised of immunization experts that is convened by the Centers for Affliction Command and Prevention. These guidelines require coverage for adults and children and include immunizations such every bit influenza, meningitis, tetanus, HPV, hepatitis A and B, measles, mumps, rubella, and varicella. An ACIP recommendation is considered to be issued on the engagement that information technology is adopted by the Managing director of the CDC.
3. Preventive Services for Children and Youth
The ACA requires that private plans cover without cost-sharing the preventive services recommended past the Health Resources and Services Administration's (HRSA's) Bright Futures Project, which provides evidence-informed recommendations to improve the health and wellbeing of infants, children, and adolescents. The preventive services to be covered for children and adolescents include some of the immunization and screening services described in the previous ii categories, behavioral and developmental assessments, iron and fluoride supplements, and screening for autism, vision impairment, lipid disorders, tuberculosis, and certain genetic diseases.
IV. Preventive Services for Women
The recommendations issued by USPSTF, ACIP, and Bright Futures predate the ACA. In addition to these services, the ACA authorized the federal Health Resources and Services Administration (HRSA) to brand boosted coverage requirements for women. Based on recommendations by a commission of the Institute of Medicine (IOM),eight federal regulations require new private plans to cover additional preventive services without cost-sharing for women, including well-woman visits, all FDA-canonical contraceptives and related services, broader screening and counseling for STIs and HIV, breastfeeding support and supplies, and domestic violence screening.
Coverage Rules and Implementation Challenges
While the ACA aims to reduce the burden of toll and increase utilise of preventive services, there are sure rules that both plans and policy holders must follow. In that location are circumstances, even so, under which insurers may charge copayments and use other forms of cost-sharing when paying for preventive services. These include:
- If the office visit and the preventive service are billed separately, cost-sharing cannot be charged for the preventive service but the insurer may still impose cost-sharing for the part visit itself.
- If the primary reason for the visit is not the preventive service, patients may accept to pay for the part visit.
- If the service is performed by an out-of-network provider when an in-network provider is available to perform the preventive service, insurers may charge patients for the office visit and the preventive service. Notwithstanding, if an out-of network provider is used because in that location is no in-network provider able to provide the service then cost-sharing cannot be charged.
- If a treatment is given as the upshot of a recommended preventive service, simply is not the recommended preventive service itself, price-sharing may be charged.ix
The Public Health Service (PHS) Human activity and federal regulations too allow plans to use "reasonable medical management" techniques to determine the frequency, method, handling, or setting for a preventive item or service to the extent information technology is not specified in a recommendation or guideline.10 While there is no formal regulatory definition or parameters for reasonable medical management, medical management techniques are typically used by plans to control cost and utilization of care or comparable drug utilize. For example, plans can impose limits on number of visits or tests if unspecified past a recommendation, cover simply generics or selected brands of pharmaceuticals, or require prior authority to learn a preferred brand drug. If a plan makes whatsoever fabric modifications that would bear on the content of the program's Summary of Benefits and Coverage (SBC) during the plan year, the plan must notify enrollees of the modify at least 60 days before it takes effect.11
The combination of these caveats and limitations has resulted in many questions virtually how plans should implement the preventive services policy. In item, questions accept arisen about the frequency, range of methods that can be used for sure services, and the types of providers that are bailiwick to the policy. The Departments of Wellness and Homo Services, Labor, and Treasury jointly issue memos as "Often Asked Questions" specifically on implementation of the Affordable Care Human activity which provide additional clarification on unlike aspects of coverage of preventive services:
- Colon cancer screening – Screening for colorectal cancer using colonoscopies receives an "A" rating from the USPSTF, yet there accept been some cases of insured asymptomatic patients being charged unexpected cost-sharing for anesthesia and polyp removal during screening colonoscopies.12 The federal government has clarified that insurers cannot impose toll sharing for medically necessary anesthesia services and polyp removal performed in connection with a preventive colonoscopy in asymptomatic individuals.13 , 14
- Aspirin for the prevention of cardiovascular disease – Over the counter medications are provided without cost-sharing only with a prescription.
- Breastfeeding – While the USPSTF recommends prenatal and postnatal breastfeeding interventions, HRSA guidelines specifically incorporate lactation support, counseling and equipment rental without cost-sharing. Federally-issued FAQs clarified that this coverage should last equally long as the woman is breastfeeding.
- Well-woman visits – The HRSA clinical preventive services for women include coverage for at least 1 well-woman preventive care visit for adult women, including preconception and prenatal care, yet controversy exists with the number of well-adult female visits that are permitted per year. The government has clarified that multiple well-womanorthward visits may exist required to fulfill all necessary preventive services and should exist provided without toll-sharing equally needed, determined by clinical expertise. Federally issued guidance notes that all dependents, including sons and daughters, must also receive all preventive services coverage as applicable, without cost-sharing. The FAQ's specifically outline that dependent daughters also receive preconception and prenatal care as function of a well-woman visit without cost sharing.
- Testing and medications for the risk reduction of chest cancer – Federal guidance reinforces the USPSTF recommendation that women with family history of breast, ovarian, or peritoneal cancer should be screened for BRCA-related cancer, and those with positive results should receive genetic counseling and genetic BRCA testing when advisable. As long as the woman has not specifically been diagnosed with BRCA-related cancer in the past, genetic screening, counseling and testing should be covered without toll sharing when the services are medically appreciate and recommended by her provider. USPSTF also recommends the provision of chemo-preventive medications for women deemed to be at high risk. As such, hazard-reducing medications, such equally tamoxifen or raloxifene, must be covered without cost sharing equally prescribed to women who are at increased risk for breast cancer and at low run a risk for agin medication furnishings.xv
- Special populations – In the cases where recommendations for preventive services, counseling, and immunizations employ merely to a certain population, such as "high risk" individuals, the authorities antiseptic that information technology is up to the health care provider to determine whether a patient belongs to the population in consideration.16 An individual's sex assigned at birth or gender identity also cannot limit them from a recommended preventive service that is medically appropriate for that private; for example, a transgender human being who has breast tissue or an intact cervix and meets other requirements for mammography or cervical cancer screening must receive those services without toll sharing regardless of sex at birth.
- Contraceptive coverage – Federal clarification states that issuers and plans must encompass the total range of prescribed contraceptive methods for women, currently at xviii distinct methods, as outlined in the FDA's Birth Control Guide. Issuers may not limit coverage to any contraceptive method, such as oral contraceptives, but must provide at least 1 version of each FDA-approved contraceptive method without cost sharing. Insurers may employ reasonable medical management inside a method, withal, to limit coverage to generic drugs and can impose cost-sharing for equivalent branded drugs. Plans are required to have an accessible and timely "waiver" procedure for patients who have a medical demand for contraceptives otherwise discipline to cost-sharing. In add-on, federal rules regarding contraceptive coverage specifically exempt or accommodate sure employers who believe that the requirement violates their religious rights.17
Bear on of the Preventive Services Rules
The federal HHS Assistant Secretarial assistant for Planning and Evaluation (ASPE) estimates that approximately 137 million people (55.6 million women, 53.5 meg men, and 28.5 million children) take received no-price coverage for preventive services since the policy went into effect.18 While the number of individuals who have gained coverage for no-cost preventive services is large, public sensation of the preventive services requirement is relatively low. In March 2014, iii and one-half years afterwards the rule took effect, less than half the population (43%) reported they were aware that the ACA eliminated out-of-pocket expenses for preventive services.xix As awareness of the benefit grows and the share of people in grandfathered plans reduces, very few privately insured individuals will have fiscal barriers to clinical preventive care. The large question remains: volition this new benefit increase use of preventive services and, ultimately, what volition be the police force's impact on the public's health and wellness care costs.
Click to view PDF
Click to view PDF
Source: https://www.kff.org/health-reform/fact-sheet/preventive-services-covered-by-private-health-plans/
Posted by: smithwhane1992.blogspot.com


0 Response to "Which Preventive Service Is Offered Free Under The Aca?"
Post a Comment